Somewhere along the way, bending down to touch your toes became a criteria for demonstrating appropriate levels of flexibility and also an essential movement for avoiding back pain in the mind of many individuals.
Often times when taking a subjective history of a patient, I have heard the phrase, “touch my toes” and whether they can, can’t, or have had a change in their ability to do that particular task.
I realize that being flexible is essential to being able to move through ranges of motion unrestricted and pain-free. And maybe because people seem to think it is ok to bend down and touch their toes as a form of stretching, it is also ok to perform this movement, repeatedly, to complete their daily activities. This isn’t the case. There are safer ways to stretch and safer ways to perform specific activities. (More on both of those in the coming weeks).
Yes, sometimes I have patients bend down in the clinic. Bending down to touch your toes, when used for assessment purposes, can help identify movement impairments. Gray Cook introduced The Selective Functional Movement Assessment (SFMA) and this movement based diagnostic system utilizes multi-segmental flexion (toe touching) as a movement pattern for those with known musculoskeletal pain. So that is not to say that we avoid the movement in the clinic completely. However, we must make it clear that assessment is not exercise and prescribing (or failure to correct) faulty movement can only lead to further injury.
So what about bending down (lumbar forward flexion) is undesirable? To reference Stuart McGill, lumbar forward flexion, even in the absence of moderate load will lead to discogenic troubles. A fully flexed position leads to strained posterior passive tissues and high shearing forces on the lumbar spine (from both reaction shear on the upper body and interspinous ligament strain). His lab work has shown this to be a good way to cause disc herniations. I read an analogy of lumbar flexion and a credit card that helps illustrate the point. If you take a credit card and bend it back and forth repeatedly, it would eventually damage and/or break. That damage doesn’t occur from a single bend, but rather a series of bends over and over.
Now consider the various activities throughout our day that might tempt us to bend through our back. There are plenty— such as wearing shoes/socks or bending down to pick an object up from the floor.
A safe alternative that I think is essential in helping to avoid injury is a hip hinge. By bending at our hips (rather than the spine), we are able to keep the spine neutral and avoid the risks of repetitive bending done daily.
Correctly performing a hip hinge, however, is easier said that done. It takes more effort, can be more time consuming, and often requires coaching and cuing to be done correctly. In my next post, I will give a short description on how to perform a hip hinge.


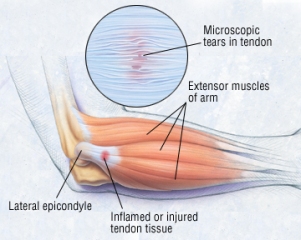
 ASTYM—The theories regarding mechanisms of action for Astym® treatment were developed based on the foundation of recent histologic research identifying the primarily degenerative nature of tendinopathies, and the investigations into the use of cellular mediators, growth factors and related products to assist in the healing and regeneration of tissues. ASTYM utilizes a series of specific movements with instruments that are run firmly along the skin following the direction of the muscle, tendon, or ligament with the goal of removing unwanted scar tissue and regenerating healthy tissue. A recent study at the American Society for Surgery of the Hand’s annual meeting showed that Astym treatment was an effective tennis elbow treatment by resolving 78.3% of chronic lateral epicondylitis (tennis elbow) cases.
ASTYM—The theories regarding mechanisms of action for Astym® treatment were developed based on the foundation of recent histologic research identifying the primarily degenerative nature of tendinopathies, and the investigations into the use of cellular mediators, growth factors and related products to assist in the healing and regeneration of tissues. ASTYM utilizes a series of specific movements with instruments that are run firmly along the skin following the direction of the muscle, tendon, or ligament with the goal of removing unwanted scar tissue and regenerating healthy tissue. A recent study at the American Society for Surgery of the Hand’s annual meeting showed that Astym treatment was an effective tennis elbow treatment by resolving 78.3% of chronic lateral epicondylitis (tennis elbow) cases.